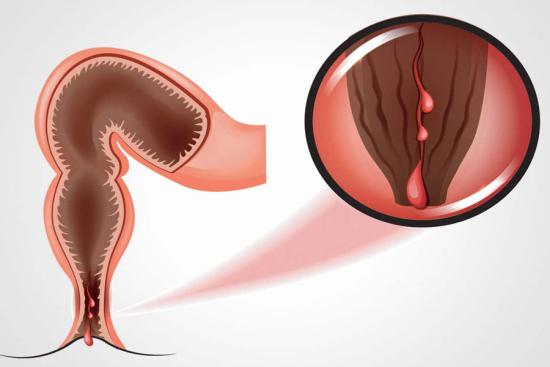
Living with recurring pain, swelling, or discomfort near the anal area can be exhausting and affect your daily life. Anal fistulas are persistent tunnels that form after infection or abscess, often causing ongoing irritation and discomfort. The good news is that with early diagnosis and proper treatment, you can find relief and regain your confidence and comfort.
With Turquie Santé, patients have access to advanced anal fistula treatments in Turkey, performed by experienced specialists in modern medical centers, ensuring effective care and faster recovery.
Risks and Side Effects
- Pain.
- Infection.
- Anal incontinence.
- Risk of recurrence.
- Oozing at the scar.
Anal fistula surgery costs in Turkey
The cost of anal fistula surgery in Turkey depends on the patient's specific case, including the type, complexity, and chosen technique. With Turquie Santé, prices are in the range of $1,800 – $3,000 USD for procedures such as fistulotomy, seton placement, or fistulectomy.
This price typically includes hospitalization, surgical fees, preoperative tests, and initial postoperative care. For an accurate assessment tailored to each patient, a personalized consultation is recommended.
Take the first step toward relief and contact Turquie Santé today to explore the best treatment options for your condition.